The placebo effect can be very large and often clinically meaningful. In IBS for example it can have up to 40% effect rate. We’ve covered some studies showing the power of the placebo effect before on Dr. Journal Club. Particularly the 3 arm trial out of Harvard on the placebo effect for IBS can be seen here. This current study research review is covering a very clever add on study to the Harvard trial.
Placebo researchers have long noticed that people seem to have varied placebo responses. Interestingly, neuroscience research points to dopamine as a possible modulator of placebo effect. The COMT enzyme is an important part of the dopamine metabolism pathway. COMT together with MAO break down dopamine in the body. There is a very well studied COMT gene variant where the protein made from this variant allele leads to the val at the 158th position becoming met. This met form of the enzyme is 3-4 fold less efficient at dopamine metabolism than the val (ancestral) form. Knowing that some people seem to be placebo responders and other don’t and with indications that dopamine may be involved in placebo responses, it seemed reasonable to these researchers to investigate whether this val158met polymorphism could be a “placebo response variant”.
The study included participants from the IBS placebo study Dr Journal Club has previously covered who gave consent for genetic screening. The researchers had the COMT val158met variant status determined for these participants. Then they looked at the IBS symptom severity score (IBS-SSS) which is a validated commonly used IBS instrument and compared the change from baseline to the end of the trial in the placebo arms in those individuals with two copies (homozygous) of the ancestral form, two copies of the val158met variant form or one copy of each (heterozygous).
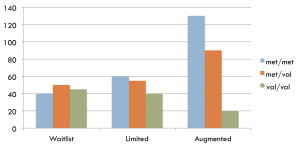
The results are indicated below in this graph. As a reminder this IBS study had 3 arms. One was a waitlist control, one was sham acupuncture with limited provider patient interaction (limited placebo) and one was sham acupuncture with a warm provider patient interaction (augmented placebo). In the original study what they found was a graded improvement effect from slight in the waitlist control, to moderate in the limited placebo group, to large in the augmented placebo group.
In this add on study what we find is that if we look at each of those 3 groups and divide the response into those with met/met, met/val, val/val we see something fascinating. In the waitlist control group, which had no placebo, we see no difference between those with different genotypes. All improve about the same. In the limited placebo group we see a slight gradation of effect with the lowest improvement seen in the val/val, intermediate in the met/val, and highest in the met/met. In the augmented placebo we see a much larger and statistically significant gradation of effect with the smallest effect seen in the val/val, intermediate in the met/val and highest in the met/met.
What this suggests is that the COMT variant can predict the placebo effect in a linear fashion depending on the number of variant alleles you have.
This is a very cool application of a genomics sub-study to a pre-existing RCT. However there remain many issues. The first is that of replication. This needs to be replicated in future trials. The other is application. If COMT does indeed predict placebo response in a clinically meaningful way, how do we utilize this in practice? I would be fascinated to hear your thoughts below. And finally it would be fascinating to do a prospective study where the intervention was given dependent on genotype and in another arm was given regardless of genotype to see prospectively if this type of “genomic medicine” approach can have an impact on clinical outcomes.
In summary, the placebo effect is fascinating and this is a fascinating study. The idea that non-specific (placebo) effects may be genetically determined is interesting. While standard RCTs try to minimize placebo effects in order to see statistical significance of the studied intervention, in clinical practice it would seem essential to use these effects to help people heal. Of course ethical issues arise, which Ted Kaptchuk’s lab, correctly, is investigating thoroughly. However, much of this effect is from a warm patient-provider interaction, which good physicians should be utilizing anyway! It is still early, but this SNP may be a quick test to determine placebo response potential, which perhaps we can utilize in our treatments.